Crisp Regional is preparing for anticipated COVID surge
Published 2:45 pm Tuesday, December 28, 2021
|
Getting your Trinity Audio player ready...
|
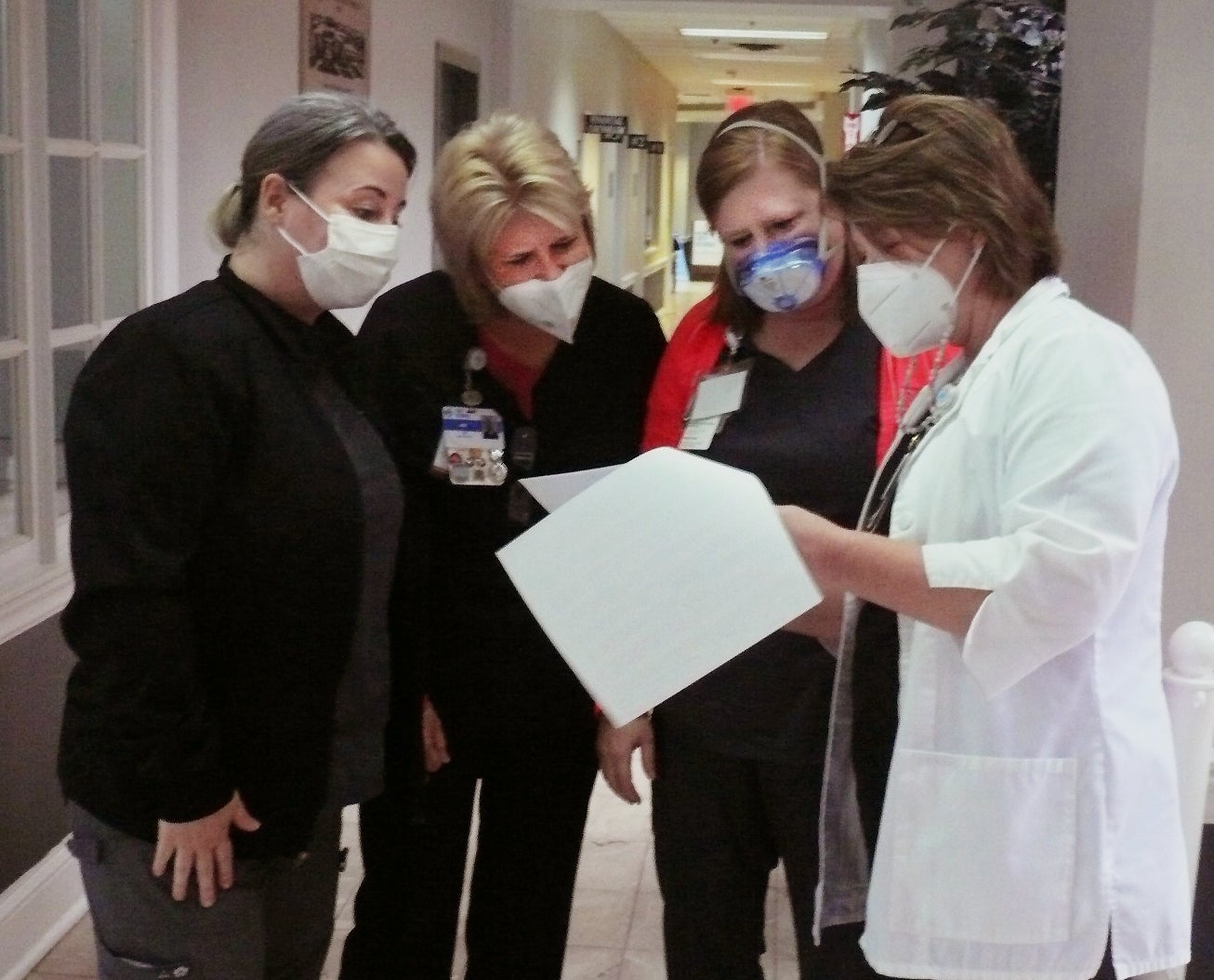
(l-r) Summer Morrow, Amy Hester and Cassandra Bellamy have a morning “huddle” with Crisp Regional Hospital’s Chief Nursing Officer, April Dukes to plan for an anticipated COVID-19 surge after the holidays. Photo by Neil B. McGahee
By Neil B. McGahee
Managing Editor
Following the Christmas holiday, the anticipated surge of COVID-19 patients, especially those infected with the Omicron variant, began coming to the hospital. But while most of the nations larger hospitals weren’t ready for the incoming patients, Crisp Regional Hospital admitted five patients — only one had been vaccinated
“What you are seeing is another big surge that is larger than the previous one,” said April Dukes, Chief Nursing Officer at Crisp Regional Hospital. “The big difference is the Omicron variant is highly, highly contagious. It seems to spread much easier but it’s not easily being translated into people being admitted to the hospital. We are also seeing a lot of young patients testing positive.
Dukes said the big surge is still coming
“I have been following our activity closely just to keep my finger on our activity. Crisp, Dooly and Wilcox counties are all in the yellow zone now, but we know what’s coming with the Omicron variant.”
Dukes said they have no way of knowing which variant the patient has contracted because the Centers for Disease Control only reveal either positive or negative results.
Viruses constantly change through mutation and sometimes the mutations result in a new variant of the virus. Some variants emerge and disappear while others like the Delta and Omicron variants persist. Since the pandemic began, the tri-counties have seen 6,278 patients admitted to hospitals and 243 deaths. In the last two weeks, nineteen have died.
The Intensive care units across Georgia are overflowing with critically ill COVID-19 patients, creating the latest crisis for hospitals trying to handle a fast-moving surge that hasn’t yet reached its peak. By last Wednesday, more than 90 percent of ICU beds were in use throughout the state.
“The last couple of days, we had very high volumes coming into our walk-in clinics and our Urgent Care and the E.R,” Dukes said. “Wait times have gotten longer and that translates into an overwhelmed staff. “
Dukes said they currently have a decent supply of testing kits, but at the rate they are being used, the supply will soon be depleted.
“We are reaching out to the federal government for help, she said”
Dukes said she thinks the worst is yet to come.
“Typically after you are exposed, it takes about three days for the symptoms to appear,” she said. “We began to see people come in about three days after the Christmas season with all the parties and the same thing will result from the New Years celebrations.”
“We meet every morning in a safety huddle — all the key directors from the hospital as well as the nursing homes. We assess our resources — how many available beds do we have; how many M-95 masks; how many gowns; how many test kits do we have. How many of our staff is positive. We are trying to stay ahead and be prepared.”


